Abstract
Background: Immunotherapy with CD19 specific chimeric antigen receptor (CAR) T cells for relapsed/refractory acute lymphoblastic leukemia (ALL) demonstrated a minimal residual disease (MRD) negative remission rate of 93% on the phase 1 portion of Pediatric Leukemia Adoptive Therapy (PLAT)-02. However, the 1-year event free survival (EFS) was 50.8%, largely due to recurrence of disease which was frequently associated with early loss of CAR T cell persistence. Subjects on PLAT-02 with <15% CD19 antigen burden in the bone marrow prior to lymphodepletion had a decreased magnitude of CAR T cell expansion and were less likely to have durable persistence of CAR T cells. Also, subjects with a rapid contraction of CAR T cells in the blood between Day +10 and Day+14, as measured by flow cytometry, had inferior long term persistence. These findings led to the hypothesis that loss of persistence may be due to decreased antigen stimulation and subsequent quiescence of CAR+ effector T cells. Episodic target exposure using T cell antigen presenting cells (T-APCs) expressing a truncated human CD19 (CD19t) could trigger CD19 CAR T cell proliferation and re-activation in vivo, resulting in more durable CAR T cell persistence and diminished risk of CD19+ relapse.
Methods: Eligible subjects for PLAT-03 (NCT03186118), a pilot study of CD19t T-APCs, must have previously enrolled on the phase 2 portion of PLAT-02 and have a stored apheresis product available. Cohorts include subjects that have an identified predictive factor to lose CAR T cell persistence early, or have already experienced early loss of CAR T cell persistence before 6 months and can receive a reinfusion of CD19 CAR T cells prior to planned T-APCs. Patient-derived T-APC products are manufactured with selected and cryopreserved CD4 and CD8 cells from the subject's original apheresis product. The T cells are activated and transduced with a lentiviral vector to express the CD19t transgene. Transduced cells are expanded in culture for 10-14 days, cryopreserved and release-tested. Subjects <25kg receive 10x106 T-APCs/kg and those ≥25kg receive a flat dose of 5x108 T-APCs. Subjects receive at least one, and up to six total doses of T-APCs at monthly intervals.
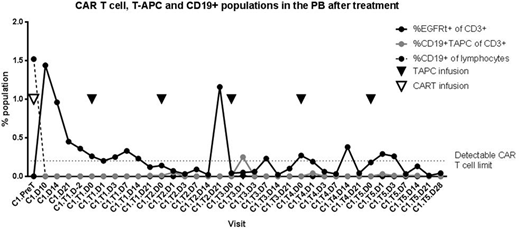
Results: Seven subjects (ages 9-23 years) have enrolled on PLAT-03; 5 enrolled based on low CD19 antigen burden at the time of lymphodepletion, and 2 based on rapid CAR T cell contraction between Days 10 and 14. T-APC products were successfully manufactured in 5/5 subjects, with two products pending manufacture. One of 5 subjects was unable to receive his planned T-APCs, as he lost CAR T cell persistence prior to T-APC infusion and failed to engraft a second infusion of CD19 CAR T cells. Of the 4 subjects that have received at least one dose of T-APCs, there have been no related adverse events (AEs) > grade 2, and no fever or cytokine release syndrome (CRS) has been observed. Grade 1-2 AEs that are at least possibly related to T-APCs have included hypogammaglobulinemia, nausea, vomiting and headache. Two subjects have completed T-APC treatment; one received all 5 available T-APC doses (subject S001), and one experienced loss of CAR T cell persistence after two T-APC doses and therefore was not eligible for further doses. Data is shown for subject S001, a 20 year old man with multiply relapsed B-ALL. He enrolled on PLAT-03 due to a low CD19 antigen burden of 4.79% by flow cytometry (inclusive of both normal and malignant CD19+ cells) just prior to lymphodepletion. He had minimal toxicity (grade 1 CRS) following CD19 CAR T cell infusion, and subsequently received 5 monthly doses of T-APCs. An increase in the quantity of detectable CAR T cells (EGFRt+ cells) was observed following T-APCs as shown below, and the subject has ongoing CAR T cell persistence at 8 months, as evidenced by B cell aplasia.
Conclusion: The first-in-human, pilot study PLAT-03 introduces CD19t T-APCs in an attempt to enhance durable CAR T cell persistence and leukemia remission following CD19 CAR T cell immunotherapy. T-APCs have been successfully manufactured from stored apheresis products collected for CAR T cell production. Four subjects have been successfully treated with at least one T-APC infusion to date, without any significant toxicity and with early evidence of efficacy. Accrual of subjects is ongoing to further assess the safety and feasibility of administering CD19t T-APCs, and to examine the impact of T-APCs on CD19 CAR T cell efficacy.
Park:Bristol-Myers Squibb: Membership on an entity's Board of Directors or advisory committees. Jensen:Juno Therapeutics, Inc.: Consultancy, Patents & Royalties, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal